Vertigo can be very complex in nature. Making the appropriate and timely referral can lead to quicker recovery times for the person. This guide will cover the strategies to help a clinician categorize vertigo-like symptoms and to assist in referring to the appropriate clinician. It is important to keep in mind that the practitioner should always err on the side of caution if they are unsure in establishing a clinical suspicion, especially since in very rare cases, vertigo can be an indication of a medical emergency and is identified through appropriate red flag screening.
Receiving further training can be a key component for improving examiner confidence when testing and ruling out red flags. This approach for navigating person care has been adapted from the Understanding Complexity of Concussion course as developed and taught by Conor Collins (2020). Within the course, there are certain differential exams (such as the HINTS+ exam) that are vital in establishing a clinical suspicion. In addition to that, Episode #45 of The Concast (2020), describes the complexity and details the different types of vertigo. This episode is a great resource as Conor talks about the etiology of the different types of vertigo.
This guide will be organized into three scenarios to be used as starting points:
- Person has symptoms that are benign paroxysmal positional vertigo-like (BPPV) in nature
- Person has constant vertigo and the HINTS+ exam is indicated
- Person has constant vertigo and the HINTS+ exam is not an indicated
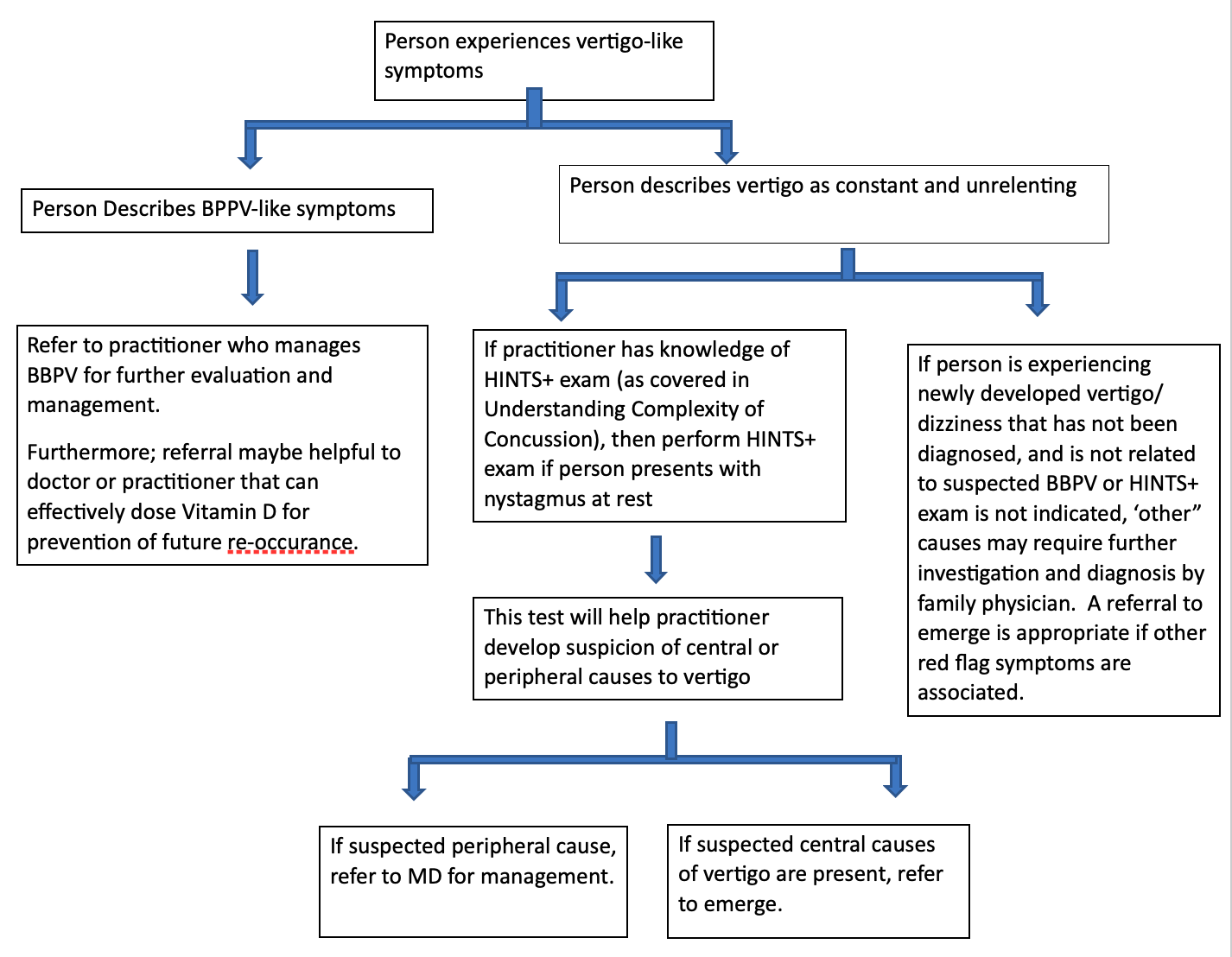
Each of these scenarios will lead to suggestions (based on clinical suspicions found) if the person should be referred to another clinician who manages BPPV, or their family physician, or if a referral to emergency care is required. In the unlikely event that a person is experiencing a medical emergency, the practitioner is equipped with the skills to identify the red flag and refer in a timely fashion. This guide is a combined hybrid approach taken after the Understanding Complexity of Concussion (2020) “vestibular management” course materials, and the flowchart (see Figure 1) that was adapted from a journal article called “clinical diagnosis of benign paroxysmal positional vertigo and vestibular neuritis” (Johns & Quinn, 2020).
First Scenario: the person describes vertigo-like symptoms as “positional dependant and short-lived”
If the person describes their vertigo to be short-lived (usually up to 20-30 seconds) and can predictably increase intensity of symptoms by positioning their head a certain way/or turning their head in a certain direction, then the therapist should be suspicious of benign paroxysmal positional vertigo (BPPV), as mentioned by Johns & Quinn (2020). For information on the etiology of BPPV it maybe be worth visiting November’s blog post as Ashley Brzezicki (2021) explores the correlation of re-occurring BPPV and Vitamin D deficiency. In this case, it is very likely to not be a medical emergency and without the presence of other associated red flag symptoms (cardiovascular, neurological, etc) no further red flag screening is required.
In this case, referring to a practitioner who specializes in BBPV treatment can greatly improve symptoms. The clinician will perform a test to identify which side and which canal is affected, then usually a maneuver is performed to force the movement of the crystals back into position. Again, this requires knowledge and training from a practitioner who is well versed in treating and managing BPPV. Usually, persons respond well to these positional techniques when performed correctly.
Furthermore, Ashley Brzezicki (2021) mentions the importance of vitamin D and its role in potentially preventing the re-occurrence of BPPV as discussed in the November 2021 blog post. In addition to referring for treatment of BPPV, it may also be of benefit for the person to consult with their doctor or another practitioner (within their scope of practice) who can prescribe and effectively dose vitamin D in prevention of future episode of BPPV.
Second Scenario: the person describes vertigo as constant and unrelenting
If the person describes their vertigo as constant and unrelenting for hours and/or days at a time and is not related to position/turning of the head, then it is unlikely that BPPV would be the primary cause of their vertigo (Johns & Quinn, 2020). In this case, further investigation may include differentiating suspicion of the peripheral vestibular system, or other central causes (i.e areas of the brain). This is where the HINTS+ exam is helpful and becomes a red flag tool to ensure that the person is not having blood flow insufficiency to areas of the brain (i.e stroke, TIA). Again, the HINTS+ exam is not used for persons with BPPV, but only to be used when a person is experiencing constant vertigo with nystagmus at rest (Johns & Quinn, 2020).
The HINTS+ exam is a great tool, however having thorough training and knowledge is foundational to performing and interpreting the exam accurately. The HINTS+ exam is also covered in the Understanding Complexity of Concussion Course. If any component of the HINTS+ exam is positive, then the person should be immediately referred to emergency care as there is a chance that a stroke may be an imminent risk. If HINTS+ exam is performed accurately and all components are negative for findings, then one may be suspicious of peripheral involvement of the vestibular system (commonly vestibular neuritis), which tends to be less worrisome compared to stroke (Johns & Quinn, 2020). A referral to their family physician would be of benefit in helping to manage their vertigo.
The HINTS+ exam includes four components, and should be only performed if constant nystagmus is observed at rest (Johns & Quinn, 2020):
- Lateral Gaze Nystagmus (bi-directional nystagmus is worrisome)
- Head Impulse Test* (normal Vestibular-Ocular-Reflex test findings are worrisome, since this is a normal peripheral finding and therefore vertigo is being driven elsewhere/likely centrally)
- Test of Skew (vertical skew during alternating cover/uncover test is worrisome)
- Hearing (abnormal hearing test is potentially worrisome)
*During the Head Impulse Test (HIT) if there is a catch-up saccade, this is less worrisome and is not likely a medial emergency. One may be suspicious of peripheral causes to vertigo (commonly acute vestibular neuritis). Even though this is an abnormal finding for the HIT, this is a favourable finding in terms of ruling out red flags including a stroke. Again, if performed correctly and an no catch-up saccade is observed (normal findings), then this is concerning and a medical emergency as this indicates that the peripheral areas of the vestibular system are functioning well, and vertigo is likely attributed to a central cause (Johns & Quinn, 2020).
One of the main components of the HINTS+ exam is the HIT. The HIT challenges the vestibular-ocular-reflex (VOR). VOR can be described as the brain’s image stabilizing software (Johns, 2021). As defined by Wallace and Lifshitz (2016, p. 153):
“Normal function of the vestibulo-ocular reflex (VOR) coordinates eye movement with head movement, in order to provide clear vision during motion and maintain balance. VOR is generated within the semicircular canals of the inner ear to elicit compensatory eye movements, which maintain stability of images on the fovea during brief, rapid head motion, otherwise known as gaze stability.”
In summary, if ANY of these components are positive when the person is experiencing vertigo in combination with constant nystagmus at rest, this warrants an immediate referral to emergency care as there are potentially central findings (Johns & Quinn, 2020).
Third Scenario: based on person conversation, vertigo cannot be categorized as BPPV, nor is the HINTS+ exam indicated, and presenting symptoms are difficult to assign a clinical suspicion
This scenario may resemble a situation where it is difficult to obtain a clinical suspicion and the HINTS+ exam is not indicated (nystagmus at rest is not evident). The individual may still require a referral to their family physician at the very least. In most cases, the person would have already sought medical attention, however in the case that the person hasn’t yet seen a doctor, a referral is very likely necessary. In certain cases, a referral to emergency care may still be warranted. As a Registered Massage Therapist, one cannot diagnose pathology, however one can develop suspicion of pathology. As best practice, one can also utilize testing criteria such as neurological and cardiovascular rule-outs to determine further suspicion of red flags. Here are some considerations that may help a practitioner when deciding if referral is warranted to either family physician or emergency care.
Considerations for Emergency Care referral:
- If vertigo symptoms are newly developed and have not been diagnosed
- If practitioner feels as though there was an element of examiner error during the HINTS+ exam and is unsure if central causes were confidently ruled out
- If cardiovascular red flags are present, including associated migrainous symptoms without prior diagnosis
- If red flags are observed while undergoing full nervous system exam (including cranial nerve exam)
Considerations for Family Physician referral (likely not an immediate emergency):
- If vertigo symptoms have been previously diagnosed and are re-occurring without presence of red flags – if symptoms are not new or worsening in nature
- If person already has received prescription medication for known diagnosis (it might be worth communicating with their family physician at the very least to let them know that re-occurring vertigo symptoms are being experienced)
- If immediate cardiovascular red flags are not present
- Red flags are not observed when undergoing full nervous system exam (including cranial nerve exam)
In summary:
Vertigo can be very complex; however, the hope is that this information could assist a practitioner in making a timely referral. The flowchart below is a visualization summarizing referral strategies mentioned throughout this blog. These are merely starting considerations and guidelines as every presentation is unique to the person and should be carefully and thoroughly assessed. Being able to identify the various types of vertigo and making the suitable referral can prove beneficial to the person.
Below: flowchart showing a hybrid adaptation of vestibular course content from Understanding Complexity of Concussion (2020) and the information acquired from Figure 1 flowchart found in “clinical diagnosis of benign paroxysmal positional vertigo and vestibular neuritis”, a journal article (Johns & Quinn, 2020).
References
Brzezicki, Ashley. “The Link between Vertigo and Vitamin D.” Conor P. Collins, 17 Nov. 2021, https://conorpcollins.com/2021/11/the-link-between-vertigo-and-vitamin-d/.
Collins, Conor P. “Understanding Complexity of Concussion.” Accessed 2020.
Wallace, J., Lifshitz, B. “Traumatic Brain Injury and Vestibulo-Ocular Function: Current Challenges and Future Prospects.” Eye and Brain, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/28539811/.
Johns, Peter, and James Quinn. “Clinical Diagnosis of Benign Paroxysmal Positional Vertigo and Vestibular Neuritis.” Canadian Medical Association Journal, vol. 192, no. 8, 24 Feb. 2020, pp. 182–186.
Johns, Peter. “How to Perform the Head Impulse Test, the Most Important Part of the Hints Plus Exam.” YouTube, YouTube, 13 Dec. 2021, https://www.youtube.com/watch?v=lkjWjFSVFGM.
“The Concast.” Dizziness and Vertigo, created by Conor P Collins, season 1, episode 45, Nov. 2020.
About the Author
Chris is a Massage Therapist and acupuncture practitioner from Ingersoll, Ontario with a special interest in managing concussion and sports injuries. While not in clinical practice Chris has served as an Instructor in Massage Therapy at the Canadian College of Massage and Hydrotherapy.
With prior education and experience as a Kinesiologist, Chris has a passion for movement and how it translates to improved patient outcomes. Whether it’s managing your symptoms virtually, or assisting students in preparing for an exam, Chris is excited to help you on your journey.


Recent Comments